Beta Bionics wants to make life easier for millions of diabetics
Nearly 80 million diabetics worldwide could potentially benefit from a new medical device being developed by the US-based medtech company Beta Bionics. And the company could be ready to launch the product on the first markets in a matter of years, founder and CEO, Ed Damiano, says in an interview with MedWatch.
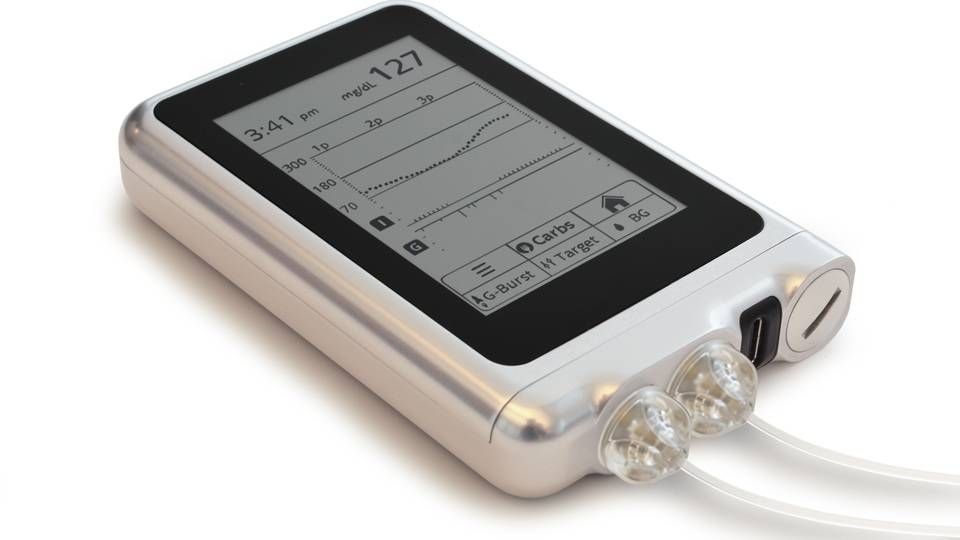
The device, known as the iLet, could become the world’s first fully automated artificial pancreas system, meant to deliver the two hormones insulin and glucagon that people with type 1 diabetes are unable to produce naturally. The device could thus be used by anyone with that disease.
But according to the CEO, it could also benefit an even greater number of people with type 2 diabetes.
“Maybe 10 percent of the type 2 population is on insulin therapy, maybe more. But even 10 percent of the type 2 population in the US - and I believe in Europe as well - is more than the number of people with type 1 diabetes in the US. And anyone on insulin therapy, we believe, could benefit from the bionic pancreas,” says Ed Damiano.
Rapidly growing problem
According to the most recent data from the International Diabetes Federation (IDF), there are now 415 million people worldwide who suffer from diabetes, and complications from the disease kills 5 million people every year.
Somewhere between five and 10 percent of the global diabetes population suffer from hereditary, autoimmune type 1 diabetes, which renders the body unable to produce insulin and glucagon. These patients need daily injections of insulin drugs.
The lion’s share of the 415 million diabetics suffer from type 2 diabetes, which is largely caused by life-style factors and slowly breaks down the body’s ability to produce and adequately use insulin. But for a smaller, but still quite significant part of that group, the disease is so advanced that the patients need insulin injections.
It is not known for sure how many of the millions of type 2 diabetics are treated with insulin, which is seen as a last resort for this population, however, some sources suggest the share could be a lot higher than 10 percent.
But going by Ed Damiano's assessment of the share of the type 2 population on insulin therapy, the market potential for his company’s artificial pancreas device could be somewhere between 58 and 79 million people. Add to this a smaller group of patients with rare conditions that cause them to overproduce insulin, such as congenital hyperinsulinism.
And the market potential is only going to increase in the future, as IDF estimates that a staggering 642 million people will suffer from diabetes in 2040.
Three settings
Once Beta Bionics’ device is fully developed it will come with three settings, allowing it to be used by three different patient populations.
One configuration will only deliver insulin and it could be used by some people with type 2 diabetes. Another setting will only deliver glucagon and that can be used by patients with diseases like congenital hyperinsulinism.
But the truly groundbreaking feature of the device will be the ability to administer carefully adjusted amounts of insulin and glucagon at five minute intervals, so patients with type 1 diabetes will finally have access to an effective replacement for their non-functioning pancreas.
“It’s constantly adjusting your insulin dosage and adapting to your ever-changing insulin needs, wherever they may take you,” Ed Damiano explains.
This is done by the help of a continuous glucose monitor from the company Dexcom and a mathematical dosing algorithm developed by Ed Damiano, which ensures that the amount of insulin or glucagon given to the patient is adapted to the person’s individual needs.
“Many people with type 2 diabetes still make glucagon and secrete it appropriately. But there are some people with type 2 diabetes who need both,” he explains.
Few years from approval
Beta Bionics is in the process of testing and refining the device and they expect to win marketing approval for the insulin-only function as early as mid-2019.
“It’s not unreasonable to think that in about 24 months from now we could have approval in both Europe and the US. I think both approvals could come around the middle of 2019. If the insulin-only system is approved in a couple of years, I’m hoping the bihormonal system will follow not too long after that,” says Ed Damiano, who pegs that approval for around 2021.

- CEO Ed Damiano hopes to be able to launch the artificial pancreas around 2021. PR photo, Beta Bionics.
Although Beta Bionics is focused on the interaction with the US FDA in its development of the iLet, the CEO does not see an approval in Europe as taking a back seat.
“Of course we are going headlong into our interactions with the FDA, but we are beginning to do this in parallel in Europe. So we are identifying notified bodies and working with European regulatory bodies to talk about clinical trial design and what needs to be done to obtain CE-marking of the device in Europe,” he says.
Clinical studies this year
The iLet has yet to be tested in clinical trials, but Beta Bionics has spent the past five years testing a prototype in in all three settings.
“The current version runs on an iPhone and it’s just an investigational device. It’s short-lived and we are going to wind that down this year and replace it with the iLet. We’ve done four and a half years of out-patient studies, testing the iPhone version of the system in all three configurations,” the CEO explains.
Beta Bionics aims to first test the insulin-only system, while a study with the bihormonal system is expected to kick off in the first quarter of 2018. Then follows the first pivotal registration study with the insulin-only function in the second half of 2018 and a similar registration study with bihormonal system should commence “shortly after that”.
“The final clinical trial for the bihormonal system will be a longer study, because you are qualifying a drug and a device – a new use for a new drug. So that’s going to involve approval from both centers in the US, the center for devices and the center for drugs,” he says, referring to the FDA’s Center for Drug Evaluation and Research and Center for Devices and Radiological Health.
The new drug that must win FDA-approval is the glucagon analogue dasiglucagon, being developed by the Danish biotech company Zealand Pharma.
Beta Bionics and Zealand Pharma have recently presented positive data from a phase IIa study, which showed that the glucagon analogue is both safe, effective and well-tolerated in a special formulation for pump use to be utilized in the artificial pancreas.
There are already a number of glucagon analogues available on the market for emergency treatment of diabetics who suffer dangerous episodes of low blood sugar known as hypoglycemia. But all of these have to be mixed on the spot before they can be given to patients.
Zealand has managed to formulate the glucagon analogue so it can easily be pumped and thus used in the Beta Bionics device.
“This product can be used in a device that can be worn for many days at room temperature or near body temperature, like an insulin pump would carry insulin,” explains Ed Damiano, adding:
“You need a stable glucagon analogue or some other way to stabilize the human glucagon molecule to be able to pump it and have it stay stable in solution for many days at room temperature and for many months under refrigerated conditions in the supply line. That’s exactly what Zealand has done.”
Investment from Novo Nordisk
Aside from having partnered with Zealand Pharma for the development of the glucagon analogue, Beta Bionics also has ties to another Danish company.
The company’s artificial pancreas system also needs insulin analogues, and these are supplied by both US-based Eli Lilly and Denmark’s Novo Nordisk. The two drug groups have also invested money in Beta Bionics.
Novo Nordisk signed a pact with the medtech company earlier this year, and the group’s US unit invested USD 5 million in its new partner at the same time. A year before that, a similar deal had been struck with Eli Lilly.
“It was very important to engage both of them and get them both at the table. Each of them made an investment in Beta Bionics that has really given us the resources to help us get to where we are over the past 18 months since we incorporated,” says Ed Damiano.
He believes the energy and productivity the small Boston-based firm exhibits with a very small staff appealed to the major drug groups.
“I think we have convinced them that we are building a system that makes their great drugs better still. They both make great drugs for type 1 diabetes management, but the quality with which those drugs are administered are very much dependent upon the user and the devices that they use,” he believes.
Moreover, the partnerships with Beta Bionics can help the pharma groups when they are to conduct new clinical trials.
“But also it’s a drug development platform, if you will, because we have this relationship with both Lilly and Novo Nordisk and we can collaborate on clinical study designs to test new drug products. So their R&D departments are really interested in the prospects that the iLet offers.”
No contact with Sanofi
But the partnerships first and foremost allow Beta Bionics to use the rapid-acting mealtime insulins Humalog from Eli Lilly and Novolog from Novo Nordisk in its device. Ed Damiano says his company is also very keen on the idea of using Novo Nordisk's insulin Fiasp, which is an even faster-acting version of insulin aspart, the active substance in Novolog.
“That’s of great interest to us as well, to make sure the iLet is compatible with that product when it becomes available more systemically. But we are working on that as well,” he reveals.
On the other hand, there seems to be no place for Sanofi’s mealtime insulin Apidra (insulin glulisine) in the artificial pancreas, once it hits the market.
“The problem with glulisine is that it has received very little market share, so for whatever reason it has not been well adopted. Glulisine is used by a very small number of people, so it hasn’t been a focus of our attention to date, and we haven’t had any interactions with Sanofi,” says Ed Damiano.
Differs from Medtronic product
While the bihormonal system from Beta Bionics would be the first of its kind, if it makes it to market, there is already one marketed device that ensures automatic insulin dosing for diabetics.
In September 2016, Irish-American medtech giant Medtronic won approval of their product Minimed 670G. That device has often been referred to in the media as an artificial pancreas, but unlike the iLet, it does not deliver glucagon. Moreover, the iLet differs from this device in a number of other ways.
“Ours is a very intuitive device. It’s not an insulin pump. It shouldn’t be confused with an insulin pump. It looks much more like a smart phone and behaves more like a smart phone in terms of ease of use and graphical user interface than a traditional insulin pump like Medtronic’s system, which looks more pager and has lots of buttons. It’s a bit more cryptic and requires some specialized training to use,” says Ed Damiano.
“In order to start the Medtronic device, you have to know something about your total daily dose of insulin, how much basal insulin you need to meet your basic metabolic requirement, how much insulin you need for meals, and how much insulin you need to take if your blood sugar is high,” the CEO adds.
He does not believe that “the dialogue between the patient and the pump” has changed significantly with Medtronic’s product, which still requires a lot of specialized knowledge that an endocrinologist would be required to provide. He does, however, expect to see a reduction in hypoglycemia from Medtronics device, once extensive data from a real-world setting is gathered. But he does not believe the device will lead to any significant reduction in long-term blood glucose.
“So I think their technology is absolutely better than anything on the market today. But our device is truly automated. You can use our device only knowing the subjects body weight. That’s it,” Ed Damiano points out and stresses:
“One big difference is that our device ultimately will use two hormones to control blood sugar, insulin to lower blood sugar and glucagon to raise it.”
Zealand announces positive results with glucagon analogue
Zealand moves US collaboration into phase II
- English edit: Martin Havtorn Petersen
Would you like to receive the latest news from MedWatch directly in your e-mail inbox? Sign up for our free English newsletter below.
Relaterede artikler
Zealand moves US collaboration into phase II
For abonnenter